-
Programs
DepartmentsAssociate DegreesBachelor Degrees
- Admissions & Aid
-
Offices & Services
Students & VisitorsHuman ResourcesInfo & Help Desk
- Blog
- Giving
- Home
- Programs & Degrees
Academic Programs
NURSING OPTIONS
Nursing


Associate of Science in Nursing (ASN)
Choose between day and evening options while earning your RN credentials.
- 2 years to complete
- In-person
- Associate degree
Nursing


LPN to RN: Advanced Placement
LPNs can earn their RN license faster with this bridge program.
- 2 years or less to complete
- In-person
- Associate degree
Nursing


Nursing: RN-to-BSN
Fast, flexible, and affordable for the working nurse.
- 16 months to complete
- 100% Online
- Bachelor degree
HEALTHCARE OPTIONS
Filter by
Healthcare
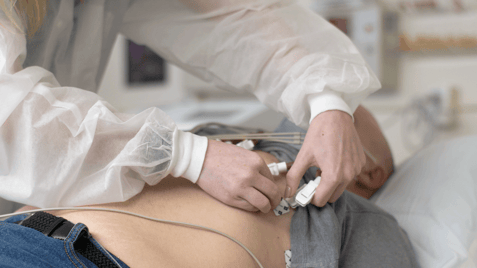
EKG Certificate
Electrocardiography training in 15 weeks.
- 4 months to complete
- Hybrid
- Certificate
Healthcare


Phlebotomy Certificate
Phlebotomy training for college credit.
- 4 months to complete
- Hybrid
- Certificate
Healthcare


Health Science
Build a strong foundation for a career in healthcare
- 2 years or less to complete
- 100% Online /or/ Hybrid
- Associate degree
Healthcare


Healthcare Administration
Take the next step toward a leadership or management position in healthcare in less than two years.
- 2 years or less to complete
- 100% Online
- Bachelor degree
Healthcare


Neurodiagnostic Technology
Change your career online in one year.
- 12* months to complete
- Hybrid
- Certificate
Healthcare


- 2 semesters to complete
- Hybrid
- Certificate
Healthcare


Respiratory Care
Respiratory therapists help patients who have difficulty breathing.
- about 2 years to complete
- Hybrid
- Associate degree
ALUMNI STORIES

“As soon as I got to Labouré, I loved the school and I loved the teachers. You’re able to ask questions. I find myself growing at Labouré.”
Victoria Browne, RN ’19
Associate of Science in Nursing Program
© 2024 Labouré College of Healthcare. All Rights Reserved.